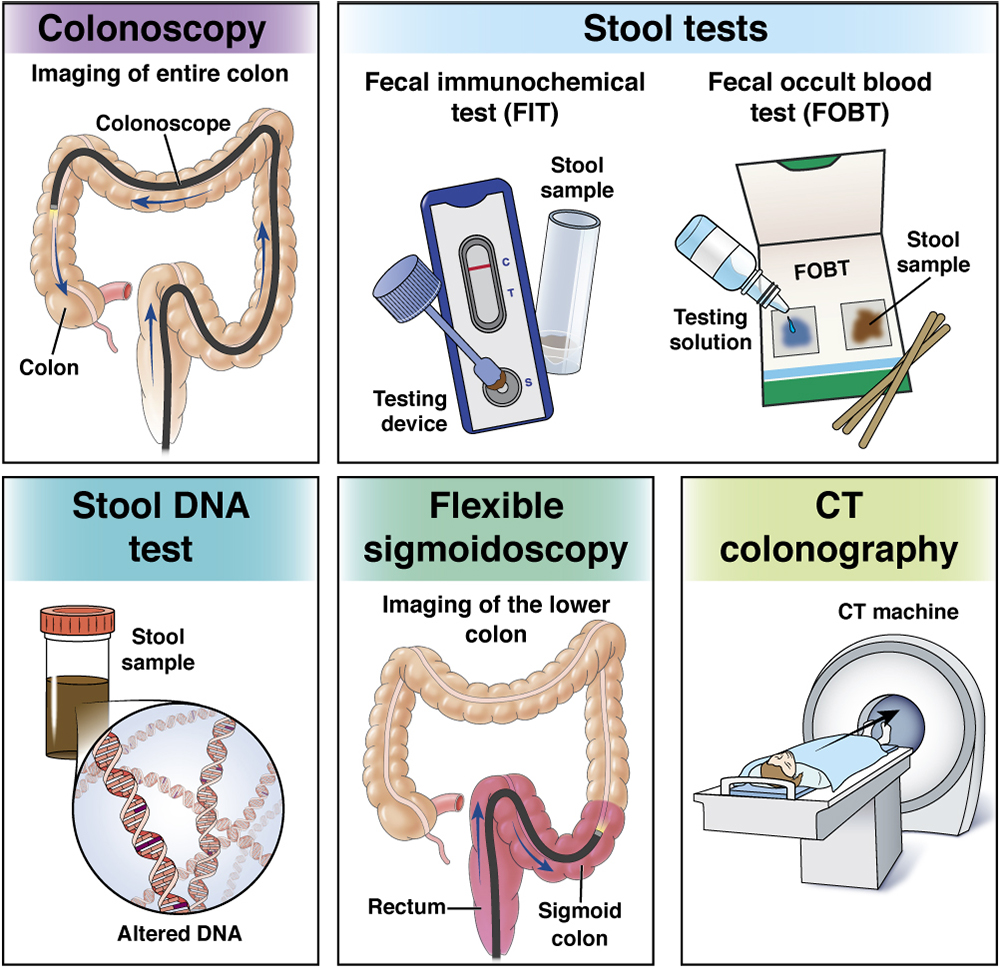
Colonoscopy
Colonoscopy is considered a first-tier method for colorectal cancer screening.
A colonoscopy involves looking at the colon from inside the body using a long, thin (about the width of your little finger), flexible tube with a tiny camera on the end, through which the doctor can view your whole colon and rectum for polyps or cancer.
- If the doctor sees any polyps during a colonoscopy, he or she will remove them right away, during the procedure.
- You will not be able to feel a polyp being removed and removing them will not impact your recovery time.
- Removing polyps during a colonoscopy could stop precancerous polyps from turning into colon cancer.
- The procedure is also able to diagnose any cancers that have already begun to grow in the colon.
This test can be done in an outpatient surgical center, an outpatient office or a hospital setting. You do not have to stay in the hospital overnight.
You will need to “prep” before this test, meaning get your body ready with a special liquid diet and laxatives the day before and day of the procedure.
You will be given medicine to make you relaxed and sleepy during this test.
You might feel some pressure during the exam, and there may be some cramping afterwards, but you most likely will not feel anything during this test.
It is the only method that blends both prevention (by getting rid of polyps that could lead to cancer) and early detection of cancer.
How often do you need a colonoscopy?
- The frequency of colonoscopy depends on personal risk and prior colonoscopy findings.
- If you don’t have a family history of colorectal cancer or prior personal polyps, colonoscopy is performed every 10 years.
- Patients at higher risk for colorectal cancer, including those with a family history or with a family or personal history of polyps, should talk to a gastroenterologist about when to start screening and how often to be screened.
How do you get ready for a colonoscopy?
- Your doctor will order you to be on a clear-liquid diet the day before your test.
- You will take laxatives and/or enemas the day before (and possibly the day of) the procedure to help clean out your colon to give your gastroenterologist a clear view.
- If you get medicine to make you relaxed and sleepy for the procedure, you will need someone to take you home and you won’t be able to go to work or drive a motor vehicle that day. The following day, most people resume their usual activities.
Fecal immunochemical test (FIT)
The fecal immunochemical test (FIT) is considered a first-tier test for colorectal cancer screening.
FIT comes in a kit with a special vial in which you can collect a small stool sample at home. Your doctor’s office will instruct you about how to perform the test.
FIT works by finding hidden, invisible blood in the stool.
FIT is low cost and pretty easy to do.

You do not have to follow a special diet or “prep” for this test.
It can find many early cancers but only the largest precancerous polyps.
If the FIT result is positive (i.e., abnormal), it means that there is blood in the stool, even if you can’t see it.
All individuals with a positive/abnormal FIT result must have a colonoscopy to look for polyps and/or cancers.
How often do you need a FIT?
- FIT must be performed annually (every year).
How do you get ready for a FIT?
- The FIT does not need a special diet or preparation.
- The FIT is available without a prescription.
Fecal occult blood test (FOBT)
Fecal occult blood test (FOBT) comes in a kit with which you can collect stool samples at home in a special container and then send them to a lab so they can look for blood in your stool.
Stool is tested in a lab for hidden blood that you cannot see.
You will need to follow a special diet before doing this test.
This test, which is pretty easy and low cost, is designed to test for early cancers, but it does not find precancerous polyps.
If the FOBT is not normal, you will need to discuss further testing with your doctor. Usually, a colonoscopy is recommended.
How often do you need an FOBT?
- Annually (every year).
How do you get ready for a FOBT?
Do not eat or use these items for two days before the test, as they may change the test results:
- Cauliflower
- Cabbage
- Horseradish
- Radishes
- Turnips
- Red meat
- Vitamin C supplements
- Foods that have iron
- Aspirin, which can irritate the stomach
- NSAIDs
FOBT is available without a prescription.

Cologuard® (Stool DNA)
Cologuard is an at-home stool test, somewhat like FIT or FOBT, that is only available by prescription.
You doctor orders the test straight from the lab, and the kit with the test is mailed from the lab to your home.
You will collect your stool in the given container, which conveniently mounts on the toilet.
You will mail back your test to the lab using a prepaid shipping label.

Cologuard finds abnormal cell parts, DNA, from colon cancers and polyps and tests for blood in your stool.
If Cologuard is not normal, you will need to discuss further testing with your doctor. Usually, a colonoscopy is recommended.
How often do you need a Cologuard test?
- Every three years.
How do you get ready for a Cologuard test?
- Cologuard does not call for a special diet or preparation.
Flexible sigmoidoscopy
This test can be done in a doctor’s office and does not need anesthesia or sedation (medicine that makes you sleepy).
For colorectal cancer screening, it is usually performed with annual FIT or FOBT.
Sigmoidoscopy is a test during which a doctor uses a short, thin (about the width of your little finger), flexible tube with a tiny camera on the end to check the rectum and the lower end of the colon for polyps and cancer. Only the final two feet of the colon’s six feet are examined.
- If the doctor sees any polyps during a sigmoidoscopy, he or she will remove them right away, during the procedure.
- You will not be able to feel a polyp being removed and removing them will not impact your recovery time.
- Removing polyps during a sigmoidoscopy could stop precancerous polyps from turning into colon cancer.
- The procedure is also able to diagnose any cancers that have already begun to grow in the colon.
Introduction of the flexible tube may be somewhat uncomfortable, and some cramping may happen during the test.
You will need to take a couple of cleansing enemas before the test and/or a gentle oral prep.
You may be given medicine to make you relaxed and sleepy during this test.
After the test, there may be some mild belly-gas pains.
If a polyp or abnormality is found, you may need a colonoscopy at a later date to examine the remaining four feet of colon.
How often do you need a flexible sigmoidoscopy?
- Every five years if annual stool tests for blood are negative.
How do you get ready for a flexible sigmoidoscopy?
- One or two mild enemas are given before the test.
Computed tomographic (CT) colonography
This test can be done in an imaging center, outpatient office or a hospital. This test will look at your colon and rectum using a special machine to take pictures.
At the start of the test, a small, flexible tube will be put into your rectum to pump air into your colon.
A machine is used to combine the pictures, making both two- and three-dimensional views that allow a trained doctor to look for polyps and cancer.
You do not need to be put to sleep for this test, but you may feel the air that is put in your colon.
You will need to clean out your colon with a laxative and/or enemas before the test, just like for a colonoscopy.
CT colonography is often performed when a colonoscopy was unsuccessful in seeing your entire colon due to technical or anatomical reasons.
If a polyp is found during this test, you will need a colonoscopy at a later date.
How often do you need a CT colonography?
- Every five years.
How do you get ready for a CT colonography?
- Preparation for a CT colonography is the same as for a colonoscopy.
- You will need to be on a special diet, usually clear liquids, the day before your test.
- Laxatives and/or enemas will be needed to clean out your colon.
- You should check with your health plan to see if they will pay for this test.
Please work with your doctor to determine the best screening options for you. Be open and honest about symptoms, concerns and questions. Remember, colorectal cancer screening has been demonstrated to be lifesaving. No butts about it: Get screened!
Blood-based screening test
The U.S. Food and Drug Administration (FDA) has approved the first blood test as a screening option for colorectal cancer. The blood test must be performed at least every three years. If results of the blood test are positive, it suggests that you may have colorectal cancer and you need to have a colonoscopy to prove the diagnosis. The blood test will not tell you if you have precancerous polyps that could turn into cancer if they are not removed.
Screening colonoscopy is the only method that blends both prevention (by getting rid of polyps that could lead to cancer) and early detection of cancer. The blood test that has been discussed in the media can only detect cancers, but not precancerous polyps.
Talk to your health care provider about whether this test is right for you.
Questions to ask your doctor
- What are my risk factors for CRC?
- What are my CRC testing choices given my past medical history?
- What are the risks and benefits of each test option?
- What happens if a polyp is found?
- How do I get ready for my test?
- What can I eat/drink before my test?
- How often should I be tested if my colon is clear?
- If a polyp is found, when should I get tested again?
- How often do you perform each test option?
- How often do you need to do a standard colonoscopy after doing a different test first?
Reviewed by

Folasade (Fola) Popoola May
MD, PhD, MPhil
Assistant Professor of Medicine, University of California, Los Angeles (UCLA), Health
Updated August 2024

Folasade (Fola) Popoola May
MD, PhD, MPhil
Assistant Professor of Medicine, University of California, Los Angeles (UCLA), Health