What is endoscopic ultrasound (EUS)?
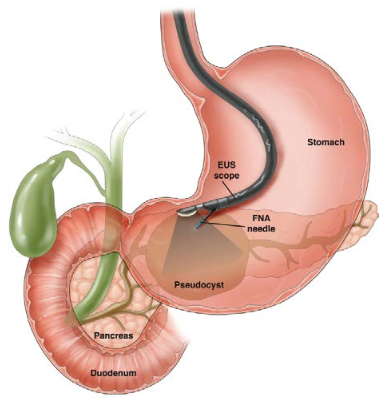
An endoscopic ultrasound (EUS) is a specialized procedure that blends:
- Endoscopy — use of a scope to look at the inside lining of the gastrointestinal (GI) tract.
- Ultrasound — use of high frequency sound waves to see detailed images of the bowel wall and nearby organs or structures.
An EUS is performed by a gastroenterologist who has advanced training.
The EUS scope is a thin, flexible tube with a camera and a light on the end. A tiny ultrasound probe is also attached to the end of the scope.
An EUS is often performed as an outpatient procedure, like other endoscopic exams.
Most EUS cases are performed with sedation (medication that helps blocks pain and makes you feel sleepy). Your doctor will talk with you about the type of sedation used for your exam. If you get sedation, you will need someone to drive you home afterward.
An upper EUS looks at the upper GI system
- Walls of the upper GI tract — esophagus (the tube that links your mouth and stomach), stomach and small intestine
- Nearby organs — pancreas, gallbladder and bile ducts
- Nearby structures — lymph nodes, tumors, cysts and blood vessels
A lower EUS looks at the lower GI system
- Bowel wall of your rectum and lower colon
- Nearby organs — bladder, prostate and uterus
- Nearby structures — lymph nodes and tumors
- Detailed images of the anal sphincter (muscles around the anus)
Fine needle aspiration (FNA)
If a tissue sample is needed, your doctor will use the ultrasound image to guide a thin needle through the endoscope to take a biopsy. You won’t be able to feel this.
Why do I need an EUS?
Your doctor may have found a lesion or abnormality at a prior endoscopy study (upper endoscopy or colonoscopy) or on an X-ray test, such as a computerized tomography (CT) scan.
An endoscopic ultrasound (EUS) will allow your doctor to see very detailed ultrasound images of the lesion or abnormality. The bowel wall and nearby organs and structures (such as lymph nodes or blood vessels) can also be seen. If a biopsy (taking a small piece of tissue to look at under a microscope) is needed, fine needle aspiration (FNA) can be performed. Your doctor will use the ultrasound image to guide a thin needle through the endoscope to take the biopsy.
Your doctor may use an EUS to:
Cancer staging describes the size of the tumor and whether it has spread to nearby lymph nodes or to other parts of the body. Staging helps your oncologist (cancer doctor) to plan the proper treatment.
- Esophageal (the tube that links your mouth and stomach), stomach, small bowel, rectal cancers.
- EUS gives very detailed pictures of the wall of the bowel. Your doctor can find out the depth of the cancer (what layers of the bowel wall are affected by the tumor) or if the cancer goes outside the bowel wall. Your doctor will also look at nearby lymph nodes and organs to see if there is any spread of the tumor.
- Pancreatic cancer.
- Lung cancer.
- Other cancers.
If you have a cancer that started in another part of your body, your doctor may use EUS to see if it has spread to sites around the bowel.
Sometimes, small lesions can be found in the wall of the GI tract with upper endoscopy or colonoscopy.
Most of these lesions are benign (not harmful), but some can be precancerous. EUS can give detailed pictures of the five layers in the wall of the bowel.
Your doctor can use EUS to find out which layer the lesion comes from and may use FNA to take a biopsy of the lesion.
To see if you have pancreatic cysts or chronic pancreatitis.
Doctors use EUS to look for lesions (masses, cysts and tumors) or gallstones.
EUS can look at the inner and outer muscles of the anal sphincter.
More uses of EUS are being developed.
Preparing for an EUS
There are important steps you must take to safely get ready for your endoscopic ultrasound (EUS). These are general instructions. Be sure to follow any instructions given to you by your doctor.
Your doctor or nurse will review the steps with you and make sure that you know how to get ready and what you can expect during and after the test. If you have any questions, be sure to bring them up with the doctor or nurse.
Getting ready for an upper EUS is not the same as getting ready for a lower EUS. Be sure to ask your doctor which test you are having and how to prepare for it.
Give your doctor a list of all the medications you are taking and any allergies you have.
- The list should include both prescription and over-the-counter (OTC) drugs, like aspirin, NSAIDs or vitamins or supplements.
- Ask your doctor before the test if any of your medications can be taken on the day of your upper EUS.
- Ask your doctor before the test if any of your medications should not be taken before your upper EUS.
- Ask your doctor before the test if you should take your medications the night before your upper EUS.
Tell your doctor if you:
- Have diabetes and what medications you are on for it.
- Are taking blood thinners or have bleeding or blood-clotting problems.
- Have a pacemaker or other implanted electromedical devices.
- Have had stomach or bowel surgery, swallowing problems or other gastrointestinal (GI) problems.
- Have heart, lung or any other health problems that may need special care before the test.
Follow your doctor’s specific instructions about what and when you can eat or drink before your upper EUS. If you do not remember the time of your appointment, call your doctor.
Do not eat any solid food after midnight the night before your test.
Do not drink any liquids or water for three hours before your test.
You may need to avoid drinking liquids for six hours before your test, depending on what medicine your doctor uses to make you relaxed and sleepy during the test.
Since you will be given medicine to block pain and make you feel sleepy (sedation), you will not be allowed to drive a car, work or make important decisions after the test.
You must have someone with you to review the discharge instructions and to drive you home after the test.
Plan to rest at home for the rest of the day after your test.
Upper EUS can be done as an outpatient procedure. Be sure you know exactly where you need to go the day of your procedure, as it may not be the same as your doctor’s office
Please follow your doctor’s instructions carefully, or you may need to reschedule your EUS for another day. Be sure to ask your doctor or nurse if there is anything you do not understand.
Give your doctor a list of all the medications you are taking and any allergies you have.
- The list should include both prescription and over-the-counter (OTC) drugs, like aspirin, NSAIDs or vitamins or supplements.
- Ask your doctor before the test if any of your medications can be taken on the day of your upper EUS.
- Ask your doctor before the test if any of your medications should not be taken before your upper EUS.
- Ask your doctor before the test if you should take your medications the night before your upper EUS.
Tell your doctor if you:
- Have diabetes and what medications you are on for it.
- Are taking blood thinners or have bleeding or blood-clotting problems.
- Have a pacemaker or other implanted electromedical devices.
- Have had stomach or bowel surgery, swallowing problems or other gastrointestinal (GI) problems.
- Have heart, lung or any other health problems that may need special care before the test.
You will need to take a bowel prep to cleanse your colon before your lower EUS.
- Typical bowel cleansing before your lower EUS can be an enema (or, occasionally, a full colonoscopy-type prep is recommended).
- Follow your doctor’s specific bowel-cleansing-prep instructions.
Follow your doctor’s specific instructions about what and when you can eat or drink before your lower EUS. If you do not remember the time of your appointment, call your doctor.
- Your diet instructions will depend on your bowel-cleansing preparation and whether or not you will receive medication to make you sleepy.
- Lower EUS is usually not painful and you may not need medicine to help you relax.
If your doctor plans to give you medicine to block pain and make you feel sleepy, you will not be allowed to drive a car, work or make important decisions after the test. You must have someone with you to review the discharge instructions and to drive you home after the test.
Plan to rest at home for the rest of the day after your test.
Lower EUS can be done as an outpatient procedure. Be sure you know exactly where you need to go the day of your procedure, as it may not be the same as your doctor’s office. Please follow your doctor’s instructions carefully, or you may need to reschedule your EUS for another day. Be sure to ask your doctor or nurse if there is anything you do not understand.
During an EUS
- A nurse will review your medical history, medications and allergies.
- You will change into a hospital gown.
- Your doctor will review the consent form for the test, answer any of your questions and ask you to sign the form, which says you understand the test being done.
- An intravenous (IV) line will be started (to give you IV fluids and medicine to make you feel sleepy during the exam).
- You will be given medicine to block pain and make you relaxed and sleepy, so you won’t feel much during the EUS.
- During the test, everything will be done to make sure that you are at ease, safe and comfortable.
- Your blood pressure, pulse and heart rhythm will be watched during the EUS. You may get extra oxygen through a nasal cannula (soft tubing).
- The doctor will use an EUS scope (a thin [about the width of your little finger], flexible tube with a tiny camera and a mini ultrasound probe at the end). The EUS scope will not block your breathing.
- You may have the back of your throat sprayed with something to numb it to lessen discomfort of the EUS scope.
- A plastic bite block may be placed between your teeth (to protect your teeth and the endoscope).
- You will lie on your left side.
- Once you are fully relaxed, the EUS scope will be carefully passed through your mouth, into your esophagus (the tube that links your mouth and your stomach) and into your stomach and duodenum, the first section of your small bowel.
- Your doctor will be able to see the EUS scope images (the inside lining of the gastrointestinal [GI] tract) and the ultrasound images at the same time.
- In some cases, the doctor may need to take a sample of tissue by fine needle aspiration (FNA). Your doctor will use the ultrasound image to guide a thin, flexible needle through the EUS scope to take a biopsy (a tissue sample that will be examined under a microscope). You will not be able to feel this.
- After the doctor is done looking inside, the endoscope will be removed and you will wake up in recovery as the medicine wears off.
- You will be given medicine to block pain and make you relaxed and sleepy, so you won’t feel much during the lower EUS.
- During the test, everything will be done to make sure that you are at ease, safe and comfortable.
- You may feel a little bloated at times, but you should feel little to no pain.
- Your blood pressure, pulse and heart rhythm will be watched during the EUS. You may get extra oxygen through a nasal cannula (soft tubing).
- The doctor will use a EUS scope (a thin [about the width of your little finger], flexible tube with a tiny camera and a mini ultrasound probe at the end).
- You will lie on your left side.
- Once you are fully relaxed, the EUS scope will be carefully passed through your anus into your colon.
- Your doctor will be able to see the endoscopy images (the inside lining of the gastrointestinal [GI] tract) and the ultrasound images at the same time.
- In some cases, the doctor may need to take a sample of tissue by fine needle aspiration (FNA). Your doctor will use the ultrasound image to guide a thin, flexible needle through the EUS scope to take a biopsy (a tissue sample that will be examined under a microscope). You will not be able to feel this.
- After the doctor is done looking inside, the EUS scope will be removed and you will wake up in recovery as the medicine wears off.
After your EUS
- When your endoscopic ultrasound (EUS) is done, you will be cared for in a recovery room until the medicine wears off and you are more alert.
- Your doctor or nurse will review the EUS results with you and give you any other details or next steps you may need.
- If a biopsy (taking a small piece of tissue to look at under the microscope) was taken, your doctor or nurse will tell you when those results will be available. They will tell you if any other testing or follow-up is needed.
- You will be told how soon you can eat and drink, plus other steps to take for getting back to your normal routine.
- Plan to take it easy for the rest of the day after your EUS. This means not driving, working or making important decisions.
- You will need to arrange to have a family member or friend listen to the discharge instructions and take you home. You should plan to resume your normal activities (driving and working) the day following your exam.
- You may feel some minor issues, such as mild sore throat (upper EUS) or mild bloating (swelling) or cramping. These should go away in less than 24 hours.
- Contact your doctor’s office if you have any questions after your EUS.
Safety of EUS
Complications from the test are rare, but can include:
- Sore throat (upper EUS) — can usually be managed with over-the-counter (OTC) lozenges or gargles.
- Bleeding.
- Reaction to the medicine given to make you sleepy.
- Infection.
- Perforation — a tear in the intestinal wall that may require surgery to repair.
- Aspiration (upper EUS) — fluid from mouth or stomach contents entering into the lungs.
- Pancreatitis (upper EUS with fine needle aspiration [FNA] of the pancreas) — inflammation or swelling of the pancreas.